Rib Fractures: Safer Dispositions
Thank you MDcalc for improving my MDM.
Isolated rib fractures—those without immediate pneumothorax or hemothorax—are common ED presentations. While the diagnosis is often straightforward, the disposition frequently is not.
The Problem: Pain (with every breath you take)
Rib fractures are exquisitely painful and notoriously difficult to manage in the ED. While regional anesthesia is effective, we often lack the immediate resources to perform blocks or must wait for IR or Anesthesia consults. Disposition is particularly challenging for older patients, where we must balance effective analgesia against the risks of respiratory depression and polypharmacy.
The Solution: Objective Risk Stratification
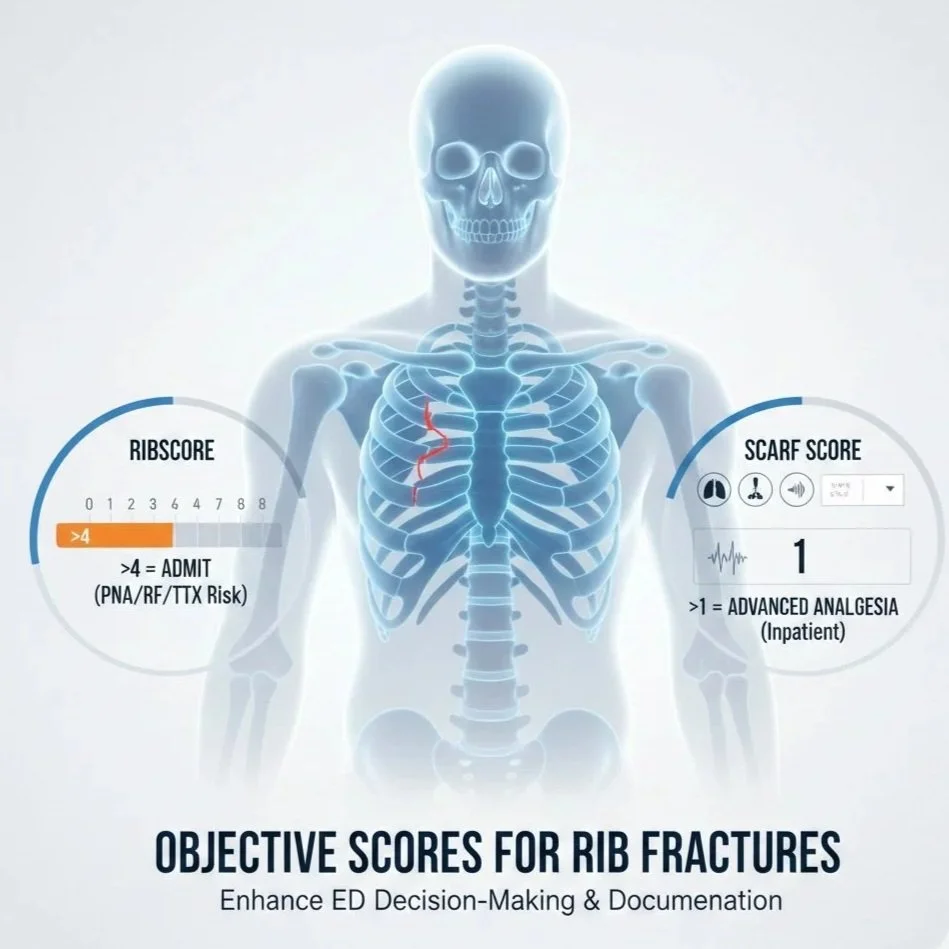
Using MDCalc, we can now utilize two objective scores to guide disposition and justify clinical decision-making.
Thanks to MDCalc, we now have 2 objective scores that you can use to help decide on disposition. Here is how I intend on integrating these scores into my treatment plans.
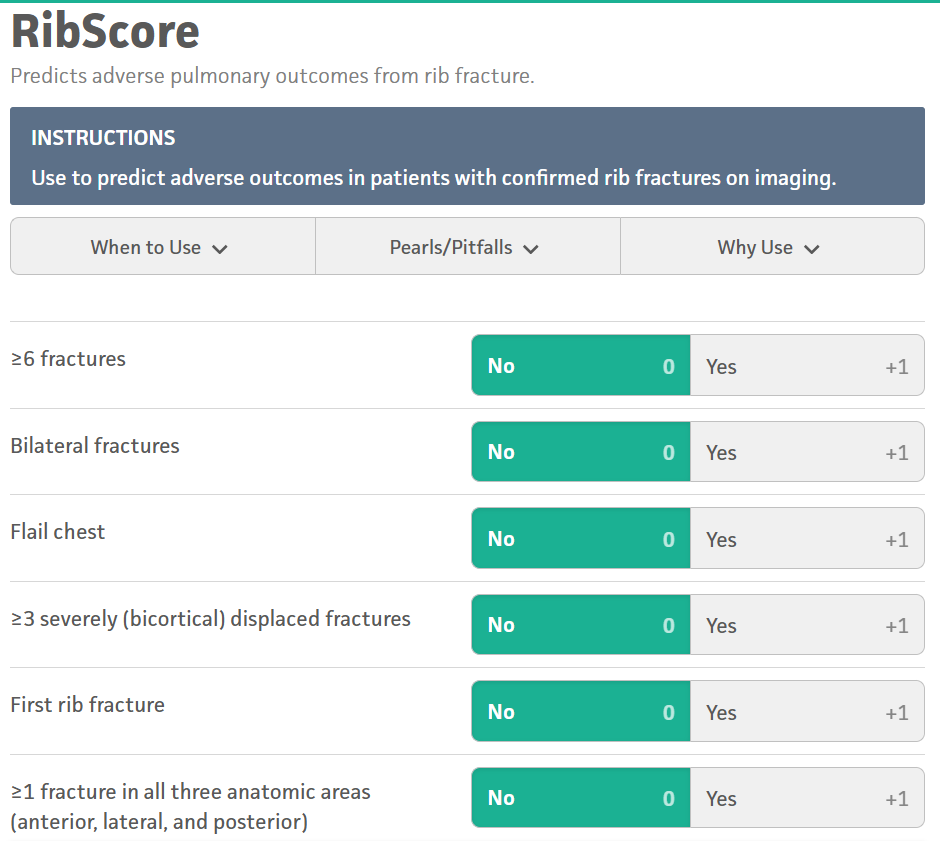
First, calculate a RibScore to predict adverse outcomes in patients with confirmed rib fractures on imaging.
Strongly consider admitting a patient with >4 points, which corresponds to a greater risk of a complication such as pneumonia, respiratory failure, and tracheostomy.
This scoring also helps justify admission and adds complexity to your decision-making in your charting.
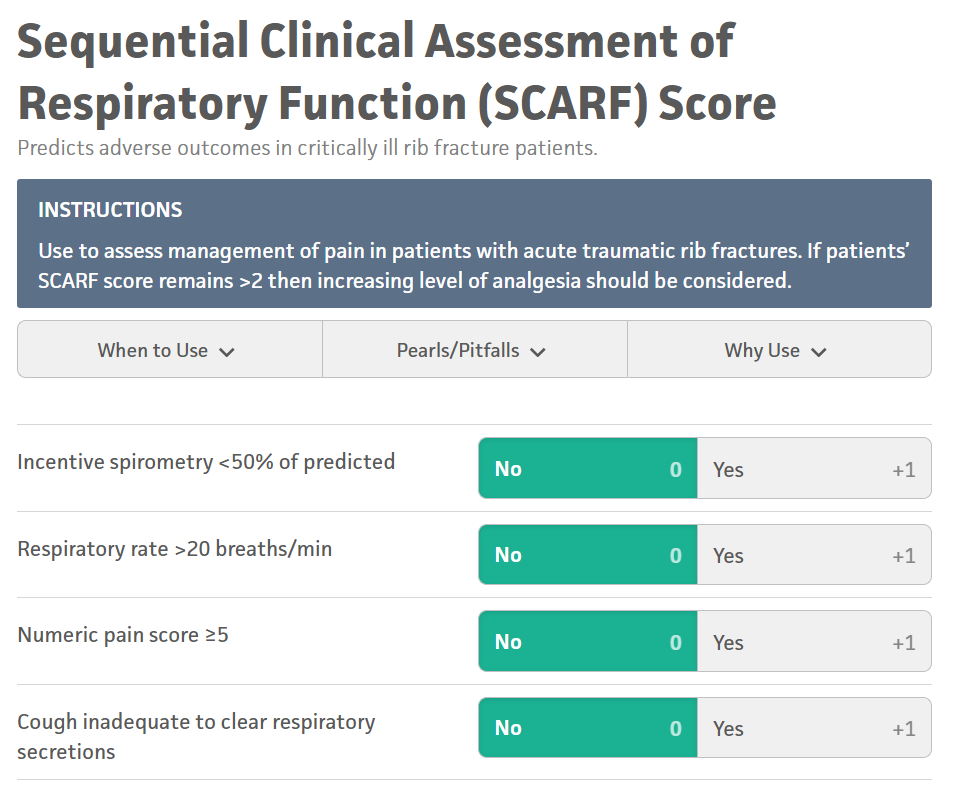
Next, a Sequential Clinical Assessment of Respiratory Function (SCARF) Score can be used to evaluate how well you are able to manage your patient’s pain in the ED prior to discharge home.
Previously, I would treat a patient’s pain with the same modality I was planning to use at home and document how they were feeling, typically after a lidocaine patch, acetaminophen, and NSAID.
Now, with a SCARF Score, I have an objective measure to add to my MDM when deciding a dispo. A SCARF score >1 predicts the need for a higher level of anesthesia, typically only available in the hospital.
According to MDCalc, when used together, the sensitivity for detecting pulmonary complications is >95%.
Expert Edge:
Add these tools to your decision-making process, but they do not replace clinical judgement. There may be many instances where patients meet admission criteria outside of any of the factors included in these scoring tools. For example, a patient may be anticoagulated, live alone, have poor respiratory reserve, or have other risk factors that make discharge potentially dangerous.
Do not ignore your gut or your patients! If your patient requires IV pain control in the ED, it is not likely that their pain is going to be controlled at home. One or both of these scores could easily justify admission, allowing you to reach a disposition much faster.
The patients most at risk are the ones you discharge! Support your decision to discharge with the RibScore, at a minimum. For "on-the-fence" patients, attempt ED analgesia and document a SCARF score <1. Should a complication arise post-discharge, your documentation will be much more defensible with these objective measures included.
Summary:
Incorporate the RibScore and SCARF score into your charting to provide an objective, evidence-based roadmap that justifies your disposition - need for admission or reasonable to discharge. By documenting these validated measures alongside your clinical judgment, you create a robust medical-legal defense beyond subjective "patient felt better" statements.
ED MDM Template: Rib Fracture Disposition
Clinical Decision Support: To risk-stratify for potential pulmonary complications, the RibScore and SCARF Score were utilized.
RibScore: [Insert Score] (A score >4 indicates high risk for pneumonia/respiratory failure).
SCARF Score: [Insert Score] (A score >1 suggests that outpatient oral analgesia may be insufficient and advanced inpatient modalities may be required).
Disposition Plan: Based on a RibScore of [X] and a SCARF score of [X], the patient’s risk for clinical decline is [Low/High].
[If Admitting]: Given the objective risk of pulmonary complications and the need for advanced analgesia (SCARF >1), the patient requires admission for pulmonary hygiene and aggressive pain management.
[If Discharging]: The patient’s objective scores support safe discharge with a multimodal oral pain regimen. They demonstrate adequate respiratory reserve and have been provided with strict return precautions for worsening shortness of breath or uncontrolled pain.
Resources & References:
For a deep dive, including a case study and patient handouts, visit REBEL EM.
Martin TJ, et al. Clinical management of rib fractures. Injury. 2019.
Chapman BC, et al. RibScore: A novel radiographic score. J Trauma Acute Care Surg. 2016.
Hardin KS, et al. The SCARF score: A dynamic pulmonary physiologic score. J Trauma Acute Care Surg. 2019.
Questions, edits, suggestions??? I am always looking to learn and improve my practice. Contact me or comment below.