My Peripheral Brain
*
My Peripheral Brain *
"I consider that a man's brain originally is like a little empty attic, and you have to stock it with such furniture as you choose. A fool takes in all the lumber of every sort that he comes across, so that the knowledge which might be useful to him gets crowded out, or at best is jumbled up with a lot of other things, so that he has a difficulty in laying his hands upon it. Now the skillful workman is very careful indeed as to what he takes into his brain-attic. He will have nothing but the tools which may help him in doing his work, but of these he has a large assortment, and all in the most perfect order. It is a mistake to think that that little room has elastic walls and can distend to any extent. Depend upon it there comes a time when for every addition of knowledge you forget something that you knew before. It is of the highest importance, therefore, not to have useless facts elbowing out the useful ones."
~Sherlock Holmes
Emergency Orthopedics - all the joints!
For more anatomical sketches from Leonardo da Vinci, click here
Orthopaedics
I particularly enjoy orthopedics (or orthopaedics if you prefer the predominant British spelling first coined by Dr. Nicolas Andry, actually a french physician, who introduced the word in his 1741 book Orthopaedia where he aimed to show methods to correct deformities in children). The word is derived form the Greek for "straight" and "child," although the field has grown beyond that of childhood fractures. My interest is primarily based on my own history of injuries, many as a child (the banner image is actually an MRI of my own knee above), and from my undergraduate study in kinesiology (the study of human movement) which I stumbled into as a nieve freshman.
In an attempt to make ortho easy, I am going to give you what you need to properly document an exam, and then from there see why you need to document and test as such in order not to miss anything (as well as pick up on some subtle diagnoses). We are going to proceed from a top down approach. I'm skipping the neck and was going to skip the low back because there are so many diagnoses that mimic back pain (AAA, renal colic, etc), but we'll include mechanical back pain for now. To go to the joint and exam you need just scroll down. Pediatric injuries have their own flavor and won't be covered here, sorry. Stay tuned to though for a true "Orthopaedia" review in the future.
Of course, there are two types of orthopedic complaints, atraumatic (mostly inflammatory like bursitis, arthritis, etc) and traumatic (fractures, dislocations, and the like). Most, but not all, important diagnoses in traumatic injuries will be seen on standard x-rays, but a good physical exam (PE) is imperative. You will also need to write a good note and actually examine the patient's neurovascular status as well as test all pertinant the tendons and ligaments. Even with all this some traumatic injuries may have normal or nearly normal x-rays, yet need surgical interventions so you will need to know these special situations. As usual, I have leaned on the internet's best teachers to show you the finer points. Thanks to all you who write and post excellent education.
The "most important" orthopaedic emergency....
...actually has little to do with the bones and more to do with the vessels and connective tissue. I'm talking about compartment syndrome. In my opinion this is the quintessential ortho emergency that you must think of on every presentation. Clinicians should have documentation to support just those thoughts. This would include things like...
Pulses/perfusion distal to the injury
Sensation normal distally
No pain on passive ROM
Muscle compartments soft
No POOP!! (pain out of proportion)
Don't miss this diagnosis by including these on every chart on every patient every time.
Compartment syndrome usually occurs after trauma such as a fracture or crush injury but it can even be chronic. It can occur anywhere that skeletal muscle is surrounded by fascia, but most commonly
leg (review the leg compartments on orthobullets.com)
forearm
hand
foot
thigh
buttock
shoulder
paraspinous muscles
From ALiEM by Dr. Katelyn Hanson
SO YOU SUSPECT COMPARTMENT SYNDROME, NOW WHAT??
Call for help. Your friendly orthopedic surgeon is the person who is going to need to treat this, if it is present with a fasciotomy
If you can, check a pressure. There is a great video provided by EM:RAP here on using a Stryker pressure monitor.
If the pressure >30 or if the Delta pressure is <30 (see illustration above), the patient is the danger zone.
Call your orthopedic surgeon for elevated pressure or low delta pressure and prep for OR fasciotomy.
So there is another “orthopeadic emergency” that is actually covered in the infectious disease section, and that is septic arthritis. Of course, patients usually present with a painful swollen joint, so you might think orthopedic injury first. Obviously, this is infectious until proven otherwise. You still might need an orthopedic surgeon for a joint washout, but I decided to put monoarticular arthritis in the ID section.
ON TO THE COMMON STUFF...
Just remember some of the most important finding on any injury is the neurovascular status. Don't only focus on the joint and x-rays. Compartment syndrome is a clinical suspicion and plain films will not show nerve or vessle injuries.
Page contents: Upper extremity orthopedics
Shoulder
Elbow
Wrist
Hand
The Shoulder
ATRAUMATIC SHOULDER PAIN:
By far and away this is going to be shoulder impingement syndrome which is really a catch all for subacromal bursitis and/or supraspinatus tendonitis. This is further discussed below. One hallmark for this is pain at night sleeping on the affected side and exam shows pain with anything that decreases the space in the subacromial area (i.e. empty can and Hawkins maneuver). Other subtle diagnoses to consider would also include proximal biceps tendonitis with pain in the same area but instead a Speed's test is positive or just resisted elbow flexion and supination (remember the biceps is the primary supinator) causes pain. If there is bruising and a Popeye arm deformity consider a biceps muscle or tendon rupture. Biceps tendon rupture can be proximal or distal so a patient may present with anterior shoulder pain and have the muscle deformity there. Patients can also have tendonitis of any of the other rotator cuff muscles (remember your SITS muscles), but this is much less common. Mostly document good movement of these muscles to assess for adhesive capsulitis. This can be done with the lift off test and resisted external rotation with arms at sides and elbows at 90 degrees. A full list of special tests can be found on Medscape.
Review your anatomy here at WebMD if you are rusty. The page also includes a list of common diagnoses.
What to document:
R or L hand dominant (arthritis/bursitis) more likely on overused side
Pain at night and with overhead movement, think impingement
Any biceps deformity or pain on exam could indicate a biceps etiology
Speed's test is for proximal biceps tendonitis and should be done while palpating the proximal tendon in the bicipital groove. It can also indicate a labral tear as this is where the long head of the biceps tendon inserts.
Empty can test decreases subacromial space and is for impingement syndrome. A painful Neer's impingment or Hawkin's test do the same.
Test internal and external rotation of the shoulder as well with the lift off test (dorsum of hand on low back and lifted off) and the resisted internal rotation with the arm abducted and elbow at 90 degrees.
Feel a radial pulse and test elbow and wrist flexion/extension
A frozen shoulder (adhesive capsulitis) will have decreased ROM passively, many other etiologies can have decreased active ROM due to pain.
What to do:
A sling is fine in the short term but can lead to frozen shoulder particularly in the elderly.
Encourage early ROM exercises like pendulum swing.
Often pain will be chronic and need a PT referral, inform patient to f/u with PCP or orthopedist if not improved with conservative measures.
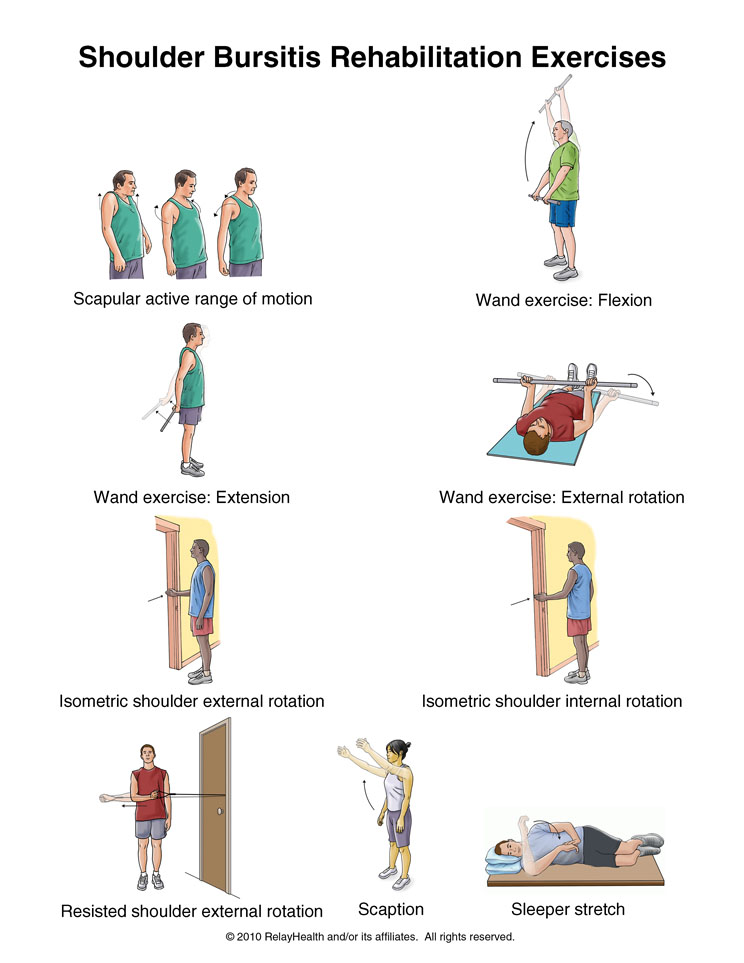
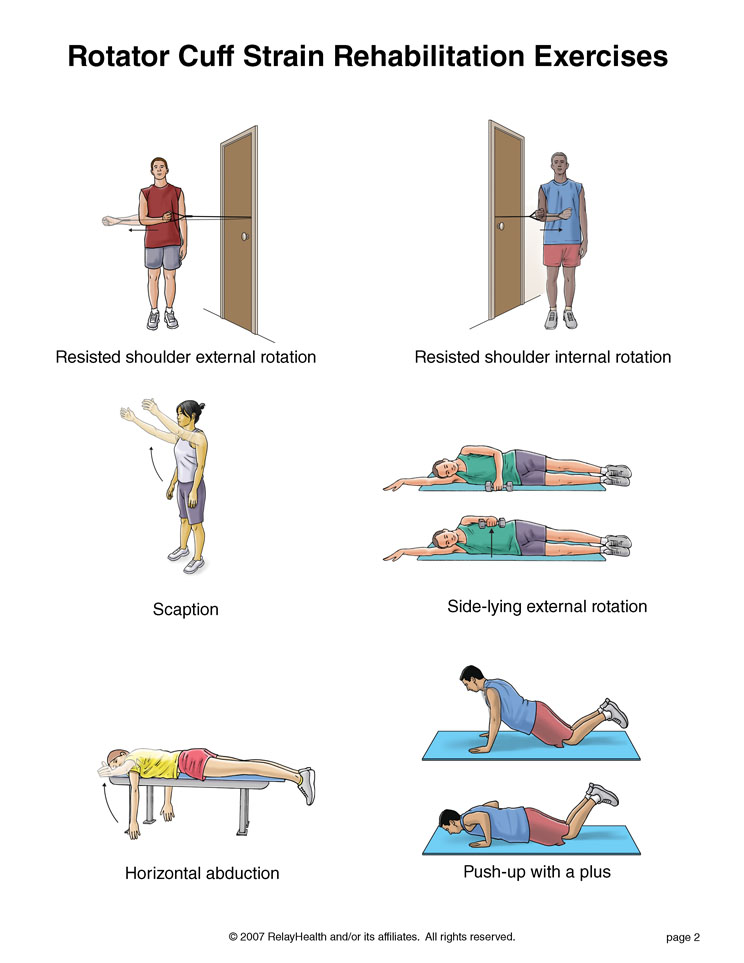
Strengthening of the rotator cuff muscles is helpful in many conditions so as long as not worsening pain with the exercises start rotator cuff muscle strengthening. This is a reasonably good educational video for patients and providers to treat impingement syndrome.
This is another great guide for shoulder rehab that you can print and send home with patients.
What not to miss:
A complete rotator cuff tendon tear. This will usually be the supraspinatus muscle and patient will not be able to abduct the first 15 degrees. They may compensate with shoulder hiking and will have a positive arm drop.
Biceps pathology such as a tear that may delay appropriate diagnosis and treatment.
Any neurologic or vascular injury.
Of course, any medical diagnosis (such as ACS) that might mimic or have associated shoulder pain. A good history and PE should clear this up so be thorough.
TRAUMATIC SHOULDER INJURY:
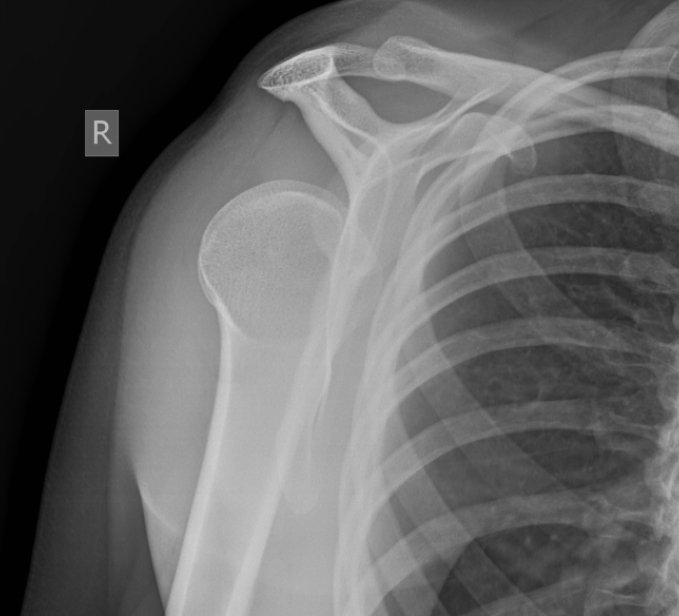
Be sure to get a Y view as pointed out by this great article on posterior dislocation on https://litfl.com/posterior-shoulder-dislocation/
It’s likely to miss an anterior shoulder dislocation, proximal humerus fracture or humoral neck fracture (BTW it's the surgical neck not the true humoral neck) on x-ray. An exception being a posterior dislocation which can be missed on just an AP view (see image right). Also because there are a bunch of different ways to reduce a shoulder, I won't go into the debate here, but just know if there are multiple ways to do something there is no one best way so find a technique and get good at it. Subtleties to these exams include documenting sensation over the lateral deltoid which shows the axillary nerve is functioning as it is often damaged with dislocation or fracture.
Of course, always document neuro and vascular status distally as the brachial artery and the arm nerves run close to the humerus. A clavicle fracture is the most common of all the traumatic shoulder injuries and should be evident on exam and confirmed on x-ray. I've never met one that couldn't go home for outpatient follow-up but check to make sure it's not an open fracture or the skin is tented and blanching and soon to be an open fracture. Those would need immediate surgical reduction.
An AC joint separation, can be difficult to pick up on plain films so consider looking at the contralateral side for comparison and if mechanism and exam is strongly indicative my be a grade I. Knowing the grades of AC joint separation not all that important as you could sling them all and send them to ortho outpatient.
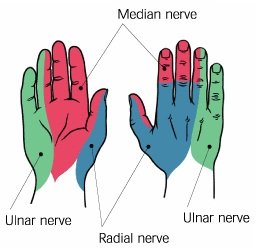
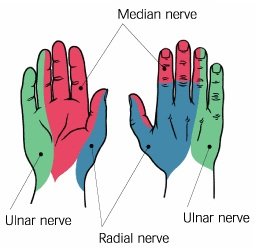
Having a quick neuro exam of the hand/fingers is a good way to ensure proximal peripheral nerve function is okay. You can make up your own or memorize this quick exam of the nerves of the arm
Radial nerve: sensation = dorsal hand, webspace between thumb and index finger; action = elbow/wrist/finger extension
Median nerve: sensation = radial border of the index finger; action = thumb abduction (thumb to index finger)
Ulnar nerve: sensation = ulnar border of the 5th finger; action = fifth finger abduction (spread the fingers)
Musculocutaneous nerve: sensation = mid lateral forearm; action = elbow flexion with supination (to isolate the biceps brachii)
Axillary nerve: sensation = over insertion of the deltoid muscle; action = shoulder abduction
Bonus: pinch the thumb on the fifth finger to assess median and ulnar nerve motor function at the same time!!!
What to document:
Complete neuro exam: discussed above
Vascular exam including distal pulses and capillary refill.
Bony tenderness or deformity (compare to contralateral side). This should include at a minimum cervical spine, spine of the scapula, clavicle, AC joint, acromium
Soft tissue deformity, or lack thereof. Classically the squaring of the deltoid with anterior dislocation.
Active and passive ROM. If any intervention such as reduction is performed document ROM before and after.
What to do:
Get X-rays duh! Probably not a good idea to try to reduce a supposed dislocation that is really a fracture.
Treat for pain. Sometimes moving the joint for radiographs and of course interventions such as reduction need appropriate pain control up to procedural sedation.
Call for expert advice in anything that you don't routinely handle. My rule of thumb is call a consultant surgeon for anyone that is going to eventually need surgery.
What not to miss:
Nerve or vascular injury. Particularly fractures can lacerate important structures like an artery. The axillary nerve (see below) is the most common nerve injury from dislocation. It provides sensation of the lateral deltoid. Document sensation here before the patient goes home (that means before and after reduction).
Secondary injury such as head or neck. If there is enough force to dislocate or fracture then perform a full physical (such as an ATLS secondary survey) to look for concomitant injuries.
Example documentation of the PE:
Musculoskeletal: The *** shoulder is *** swollen or deformed on inspection. The range of motion is full/limited to *** because of the pain. There is good abduction without shoulder hiking and no arm drop when compared to the contralateral side. There is *** tenderness of the clavicle, a.c. joint, or spinous scapula. There is *** tenderness inferior to the acromion in the area of the supraspinatus tendon and bursa. Empty can test is ***. Hawkin's test and Neer impingement test is ***. Speed's test is ***. There is *** internal and external rotation as tested by lift off and resisted external rotation with arm in adduction. Sensation intact over the lateral deltoid and down to the fingertips including the palm and dorsum of the hand. Positive radial pulse. Normal range of motion and 5+ strength to flexion and extension of the wrist and elbow. Fingers are warm and well perfused with good capillary refill.
The Elbow
ATRAUMATIC ELBOW PAIN:
Most often this can be diagnosed in 30 seconds with point tenderness and resistance of wrist flexion and extension. This is because the most common tendonitis or overuse injuries at the elbow are actually the insertion of the common flexor and common extensor tendons of the wrist and hand. Medial epicondylitis (i.e. Golfer's elbow) is tenderness at the medial epicondyle and pain there with resisted elbow flextion, while lateral epicondylitis (Tennis elbow) is pain at lateral epicondyle with palpation and resisted wrist extension. No x-rays are required and wrist splinting with pressure bands at the proximal tendon with ice and NSAIDs are the treatment of choice. Of course, the biceps and triceps tendons can have tendonitis and this is demonstrable on exam as well. There will be tenderness of these tendons and pain with resisted movement. The triceps is responsible for elbow extension and the biceps brachii can be isolated by having the patient flex the elbow and supinate against resistance (I grasp their hand like a handshake to add resistance). Sometimes olecranon bursitis results without trauma or very mild trauma and is again easy to see, palpate, and diagnose. Much consternation arises with aspiration of these bursa or not, so I will duck out of the debate and say that rarely would I aspirate because those whom I am concerned have a septic bursa look like there could be overlying cellulitis and I don't want to seed a sterile inflamed bursa. Call your local orthopedist for advice.
What to document:
R/L handedness and any repetitive movement in occupation or recreation that could cause the symptoms.
Specific location of the tenderness and what elicits the pain as a epicondylitis can be subtlety different from a biceps or triceps tendonitis.
Always the vascular status distally (i.e. radial pulse)
Always the neuro function at the joint and distally.
What to do:
Test for elbow pain with wrist flex/extension. As mentioned the common flex/ext tendons insert at the elbow.
X-rays are rarely absolutely necessary but do add to the diagnosis as sometimes you could catch an avulsion fracture
Start NSAIDs and ice. This usually will dramatically decrease pain. I like to have patients freeze small paper cups of water and rub them on the areas of pain.
What not to miss:
A full tear of the distal biceps. Flexion can be achieved with the brachioradialis so assess in full supination and with resisted supination compared to the contralateral side. Long term tendonitis or medications can weaken the tendon making the full tendon tear a relatively atraumatic event.
Same can be said for triceps tendon tear. Be sure to take gravity out of the equation when testing the triceps strength. Thankfully this is the only extensor.
Example PE for epicondylitis:
Musculoskeletal: The *** elbow is exquisitely tender over the *** epicodyl. Full flexion and extension of the elbow. Wrist flexion and extension exacerbates the pain but is intact. No tenderness over the olecranon or triceps brachii tendon. No swelling of the olecranon bursa. The shoulder is not swollen or deformed on inspection and range of motion is full. There is no bony tenderness along the radius or ulna distally. Sensation intact over the lateral deltoid and down to the fingertips. Positive radial pulse. Normal range of motion and 5+ strength to flexion and extension of the wrist and elbow. Fingers are warm and well perfused and sensation intact.
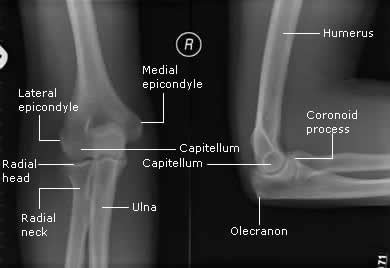
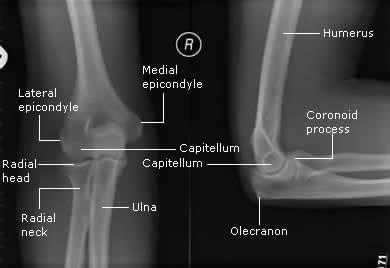
A review of the bony features of the elbow.
TRAUMATIC ELBOW INJURY
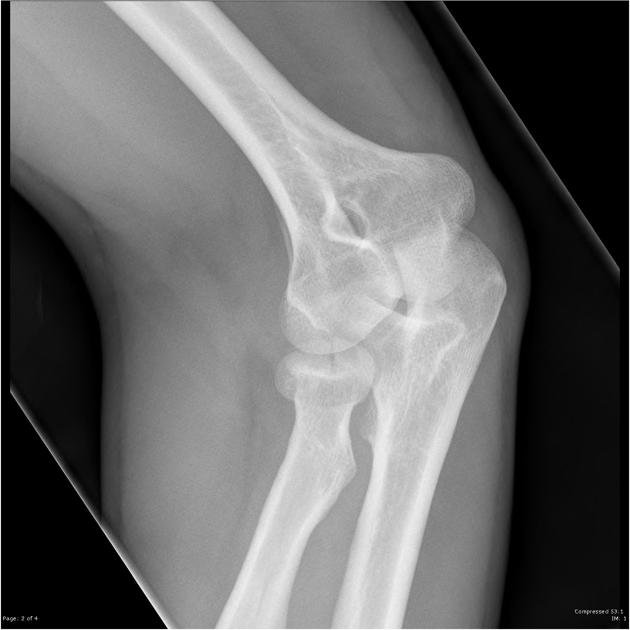
Most commonly from a FOOSH (fall on outstretched hand) injury, the radial head fracture is the winner of the most common injury in this joint. With the aforementioned mechanism and tenderness over the radial head (and pain with pronation/supination), have a low threshold to diagnose with occult fracture (even if one is not seen on plain films). As seen below, the presence of a posterior fat pad or sail sign indicates swelling (in this case bleeding) into the joint capsule and could indicate a radial head fracture and thus should be treated as such until proven otherwise. By way of review, a posterior fat pad seen on lateral films is never normal and an anterior fat pad can be normal but shouldn’t be a large triangle like a sail anteriorly. Little did I know, but you can also get a radial head-capitellum view plain x-ray in addition to standard views to pick up a few more radial head fractures not seen on initial films. Plain films are not perfect so splint all your patients with a strong likelihood of radial head fracture by history, exam, and/or x-rays in a long arm splint at 90 degrees flexion down to the wrist to prevent pronation and supination. These patients should be seen by ortho urgently as they might need surgery.
Radial head capitellum view, aka 45 degree radial head view from http://www.wikiradiography.net/page/Imaging+Radial+Head+Fractures
Other traumatic injuries include olecranon fracture and elbow dislocation. Both are easily seen on x-rays. The former occurs usually with a fall directly onto a flexed elbow (the x-ray finding and exam is obvious) and the latter takes substantial force to dislocate this relatively stable joint (and it takes a fair amount of force to reduce as well).
I have found the technique to the right to be the most effective, but if less muscle mass the other techniques would work.
What to document:
R/L handedness
Mechanism of injury
Radial pulse and capillary refill distally
Neuro exam of the wrist and hand
Bony tenderness or deformity of the medial/lateral epicondyl, olecranon, radial head and down the radius and ulna to the wrist.
What to do:
Splint fractures and suspected fractures at 90 degrees flexion. Per usual check and document neurovasc status after application
Provide pain relief up to procedural sedation for elbow reduction
What not to miss:
Test the radial, ulnar, and median nerves separately (see above) as they all cross the joint and could be injured in trauma
Feel radial pulse distally and consider an Allen test for possible ulnar artery injury.
Always think potential compartment syndrome and look for signs as well as warm patient of symptoms and when to return for a recheck.
Example PE for elbow trauma:
Musculoskeletal: The *** elbow has *** deformity. There is bony tenderness over the ***. Flexion and extension of the elbow is limited to ***. Strong wrist flexion and extension. No swelling of the olecranon bursa. The shoulder is not swollen or deformed on inspection and range of motion is full. There is no bony tenderness along the middle and distal radius or ulna. Sensation intact over the lateral deltoid and down to the fingertips including the palm and dorsum of the hand. Positive radial pulse. Normal range of motion and 5+ strength to flexion and extension of the wrist and fingers including finger adduction and abduction with good opposition of the thumb. Fingers are warm and well perfused and sensation intact.
The Wrist
ATRAUMATIC WRIST PAIN
Not a common complaint. Think tendonitis. Some people might have a ganglion cyst easily palpated on exam. Carpal tunnel impingement occurs in the wrist but usually presents with hand symptoms. Ask about previous fractures or surgeries because a change in anatomy can be a set up for tendon irritation. Most of the common tendonitis presentations will be discussed below in the hand section.
TRAUMATIC WRIST INJURY
Frequently quoted to be the second most common fracture, a distal radius fracture is by far the most common fracture I see in the ED (maybe all those clavicle fractures get seen in the PCP's office). This fracture comes in many types depending on the mechanism and age (i.e. fragility) of the patient. Common types include: Colles', Smith's, dorsal and volar angulated Barton's (line one below), Die-punch, Chauffeur's, and ulnar styloid (line two plus an impacted intra-artciular comminuted distal radius and ulna styloid fracture) to name a few. And this is excluding the common pediatric greenstick or torus fractures. Of course, any fracture should be described thoroughly as intra or extra-articular, angulated, impacted, and/or displaced. All of the following images are form The Radiology Assistant and while in a little more depth than you may need, I think it is worth a read.
Practice finding your own navicular in the snuffbox by placing your thumb there and ulnar deviating the wrist a bit.
Most wrist injuries are going to come in after a FOOSH. Obviously all the above fractures are named after their radiographic findings so you will not miss them, but you can miss a particularly dangerous fracture, the occult scaphoid (aka navicular) fracture, because it does, by definition, not show up plain films. Therefore, you must press on the anatomic snuffbox of every patient after a FOOSH (I document this on every fall even without wrist pain).
While the sneaky scaphoid fracture gets a lot of attention, there can be other carpal bones injured in FOOSH injuries. In particular, pain at the hypothenar side (opposite the scaphoid) can be a fracture of the hook of the hammate or pisiform fracture. Ever get a carpal tunnel view? Me neither, but the next time I see a patient point tender over the carpals at the base of the hypothenar hand I will get this view. For more about a hook of hamate fracture, check out orthobullets. I didn’t know these often come with direct trauma from a bat or golf club held over this vulnerable bone.
Learn more about the Terry Thomas sign - https://litfl.com/terry-thomas-sign/
What to document:
R/L handedness
Radial pulse and capillary refill of all digits
Median, radial, and ulnar nerve sensation (two point discrimination) and motor function
Any gross deformities
Snuffbox tenderness, or lack thereof
Elbow and shoulder exam as discussed above, especially the radial head which can also have an occult fracture so press on it!
What to do:
Get x-rays for trauma as usual
Call ortho for any displaced or open fractures that will need the OR
Use the contralateral, uninjured snuffbox as a guide to true tenderness. This exam is not comfortable at baseline.
Think about special x-rays (like carpal tunnel view for hypothenar wrist tenderness or the clenched fist view for scapholunate dissociation).
When in doubt splint and re-radiograph in a week or two. This is usually the way a true navicular fracture is found and there are some subtle variations of fractures, particularly intra-articular that can be missed initially and cause problems down the road.
What not to miss:
Compartment syndrome! This should run through your mind on any and every fracture. The forearm and hands are more common places for compartment syndrome.
Occult scaphoid/navicular fracture. I think I've said snuffbox enough. Make sure it ends up on your charts.
Example PE for traumatic wrist injury:
*** Arm: There is swelling and tenderness of the distal radius and *** obvious deformity of the distal forearm. The skin is intact. Flexion, extension, adduction, abduction of the fingers and thumb including opposition is intact. The fingers are warm and well perfused with good capillary refill. Full range of motion of the elbow without pain. Full range of motion of the shoulder without pain. Clavicles are nontender bilaterally.
All other joints demonstrate normal exams
The Hands
ATRAUMATIC HAND PAIN
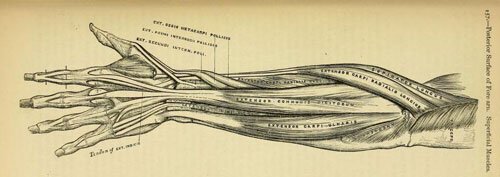
Not a lot of atraumatic hand pain complaints coming to the ED. The hands are a focal area for soft tissue infections, but that belongs more in different lecture. As for musculoskeletal problems, of course, any joint or tendon can develop arthritis or tendonitis, and this will be evident on exam. Osteoarthritis will rarely present to the ED, and rheumatoid or gouty arthritic patient's usually carry this diagnosis with them. Any tendon can also be irritated and cause pain. A review of the many tendons is seen below.
The extensor pollicus longus and brevis are two of the more common tendons (and sheaths) aggravated by repetitive microtrauma. This inflammatory process is so common that it gets its own special name of de Quervain's tenosynovitis (see a great review article at Medscape) and its own set of equally esoteric maneuvers (which I commonly confuse) named the Finkelstein and Eischoff tests. For a quick review of these check out this wikipage.
There is one more relatively common atraumatic hand presentation not discussed. See if you can guess by the example documentation below. For a review of this topic click here.
Example PE:
*** Arm: Skin is intact with no ecchymosis or erythema. Normal movement of all of the joints of the hand including adduction, abduction of the digits, flexion and extension of all of the joints of the fingers with good thumb opposition to the 5th finger. No atrophy over the greater thenar eminence. Sensation intact over the radial, ulnar, and median nerve distributions. Capillary refill <2 seconds at all fingertips. *** Tinnel's test over the wrist with a positive Phalen maneuver after about 30 seconds. No wrist or elbow tenderness with full ROM of theses joints.
TRAUMATIC HAND INJURIES
(If you have worked in EM for any period of time, you have seen a lot of cuts and crush injuries to the hands and fingers. Most important here is to look for nerve and/or tendon injuries. This is a fundamental of all wound evaluation but especially important on the hand because the tendons and are so close to the surface making them easy to injury and if injured and not repaired or healed properly can result in major disability. Obviously every hand injury should be explored through the full ROM of all the joints at or distal to the wound.
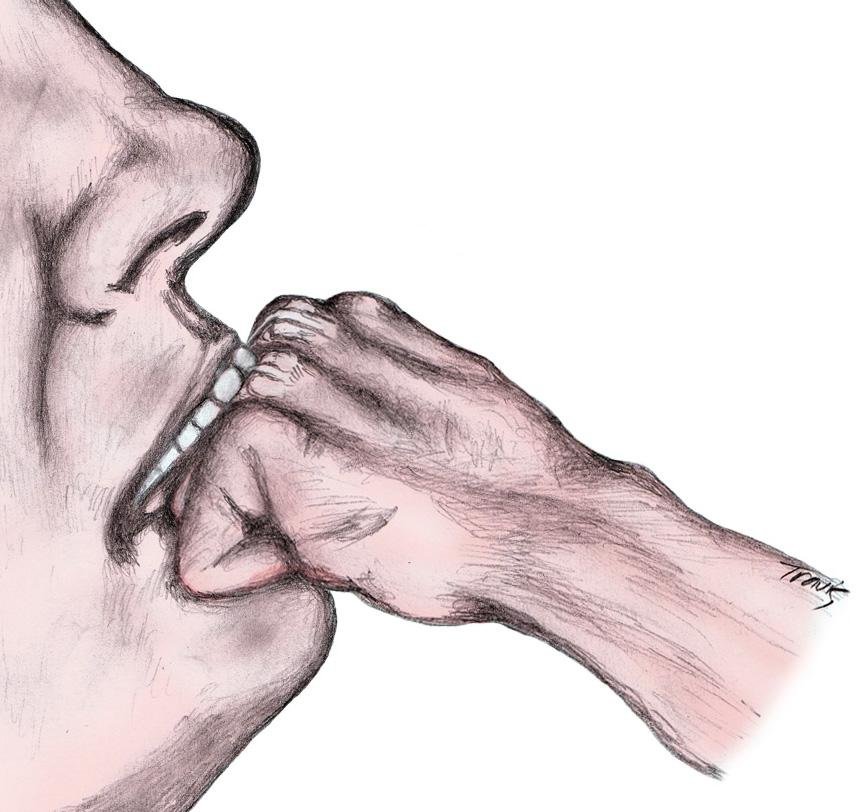
The best illustration of this is the fight bite injury. This occurs as illustrated and can injure the skin, extensor tendon, and open the joint. All can then be exposed to oral flora that can result in devastating infections. Make sure to examine these and other similar injuries through the full ROM to see if and where the extensor (or in other cases, the flexor) tendon is injured and if the joint space is invaded it likely needs a washout in the OR.
Other extensor tendon injuries are also very common in the ED. All of these are discussed at ALiEM, and is a great review of more information than can fit here. One thing to highlight is the Elson's test for extensor hood injury. This is easily missed but can lead to a permanent boutonnierres deformity. Check out the video below and lacerationrepair.com for more.
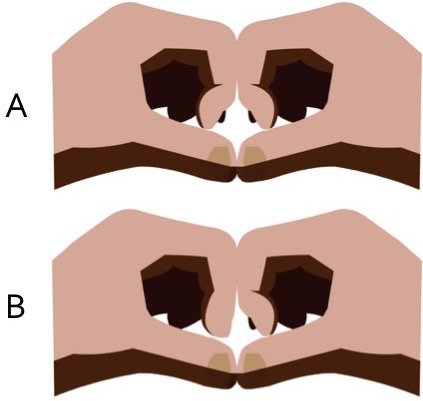
The modified Elson test from Dr. Brian Lin. Try it on yourself! A is normal: B is abnormal
Other trauma can result in closed tendon rupture or joint dislocation. Commonly the PIP joint is dislocated dorsally and can be reduced with axial traction easily. A volar dislocation is less common and causes more injury. Both should be splinted volar dislocation definitely sent to hand surgeon (this site provided the picture and the advice).
A mallet finger is a rupture of the extensor tendon at the DIP joint (thanks to 3pointproducts.com for the picture and you can see a type of splint you can use for this) and a jersey finger is rupture of the flexor digitorum profundus (this site provided the picture and some good patient info) and both can have associated avulsion fractures so always get x-rays, splint, and send to hand specialist. A gameskeeper or skier's thumb is a torn ulna colateral ligament of the MCP joint of the thumb (thanks again 3pointproducts.com). This injury is special because unlike other ligament injuries around the joints of the hand, it may not heal without surgery and can lead to a weak grip.
If any teenage boy presents with "atraumatic" pain and swelling over the 5th metacarpal, get an x-ray regardless. They might just be lying because mom is in the room. https://radiopaedia.org/cases/boxer-fracture-19
There are so many more ways to injure a hand, I don't have time to mention them all. Lastly I will show you the boxer's fracture. Quiz yourself on this at one of my favorite sites lifeinthefastlane.com, and thanks for the radiography.
Exam PE:
Extremities: There is tenderness over the 4th and 5th metacarpals of the *** hand. There is no laceration or bleeding. There is *** ecchymosis and swelling. Flexion and extension of all of the fingers is full and strong but pain with extension of the 4th and 5th fingers. There is normal finger cascade. Patient is able to flex and extend, abduct and adduct all of the fingers and thumb including good opposition of the thumb. Sensation and capillary refill intact distally. No other injuries.
Emergency Ortho: Wrist
Gaglion cyst courtesy of The Hand and Wrist Institute that has a good review here.
ATRAUMATIC WRIST PAIN
Not a common complaint. Think tendonitis. Some people might have a ganglion cyst easily palpated on exam. Carpal tunnel impingement occurs in the wrist but usually presents with hand symptoms. Ask about previous fractures or surgeries because a change in anatomy can be a set up for tendon irritation. Most of the common tendonitis presentations will be discussed below in the hand section.
TRAUMATIC WRIST INJURY
Frequently quoted to be the second most common fracture, a distal radius fracture is by far the most common fracture I see in the ED (maybe all those clavicle fractures get seen in the PCP's office). This fracture comes in many types depending on the mechanism and age (i.e. fragility) of the patient. Common types include: Colles', Smith's, dorsal and volar angulated Barton's (line one below), Die-punch, Chauffeur's, and ulnar styloid (line two plus an impacted intra-artciular comminuted distal radius and ulna styloid fracture) to name a few. And this is excluding the common pediatric greenstick or torus fractures. Of course, any fracture should be described thoroughly as intra or extra-articular, angulated, impacted, and/or displaced. All of the following images are form The Radiology Assistant and while in a little more depth than you may need, I think it is worth a read.
Colles Fracture
Smith fracture
Dorsal angulated Barton fracture from https://radiologycases.my/2020/03/31/barton-fracture/
Volar angulated Barton (aka Reverse Barton) fracture from https://litfl.com/barton-fracture/
Die-punch fracture from https://radiologyassistant.nl/musculoskeletal/wrist/fractures
Chauffuer wrist fracture
Ulnar styloid fracture
My own snuff box
Most wrist injuries are going to come in after a FOOSH. Obviously all the above fractures are named after their radiographic findings so you will not miss them, but you can miss a particularly dangerous fracture, the occult scaphoid (aka navicular) fracture, because it does, by definition, not show up plain films. Therefore, you must press on the anatomic snuffbox of every patient after a FOOSH (I document this on every fall even without wrist pain).
Terry-Thomas sign of scapholunate dislocation from https://litfl.com/terry-thomas-sign/
While the sneaky scaphoid fracture gets a lot of attention, there can be other carpal bones injured in FOOSH injuries. In particular, pain at the hypothenar side (opposite the scaphoid) can be a fracture of the hook of the hammate or pisiform fracture. Ever get a carpal tunnel view? Me neither, but the next time I see a patient point tender over the carpals at the base of the hypothenar hand I will get this view. For more about a hook of hamate fracture, check out orthobullets. I didn’t know these often come with direct trauma from a bat or golf club held over this vulnerable bone.
What to document:
R/L handedness
Radial pulse and capillary refill of all digits
Median, radial, and ulnar nerve sensation (two point discrimination) and motor function
Any gross deformities
Snuffbox tenderness, or lack thereof
Elbow and shoulder exam as discussed above, especially the radial head which can also have an occult fracture so press on it!
What to do:
Get x-rays for trauma as usual
Call ortho for any displaced or open fractures that will need the OR
Use the contralateral, uninjured snuffbox as a guide to true tenderness. This exam is not comfortable at baseline.
Think about special x-rays (like carpal tunnel view for hypothenar wrist tenderness or the clenched fist view for scapholunate dissociation).
When in doubt splint and re-radiograph in a week or two. This is usually the way a true navicular fracture is found and there are some subtle variations of fractures, particularly intra-articular that can be missed initially and cause problems down the road.
What not to miss:
Compartment syndrome! This should run through your mind on any and every fracture. The forearm and hands are more common places for compartment syndrome.
Occult scaphoid/navicular fracture. I think I've said snuffbox enough. Make sure it ends up on your charts.
Example PE for traumatic wrist injury:
*** Arm: There is swelling and tenderness of the distal radius and *** obvious deformity of the distal forearm. The skin is intact. Flexion, extension, adduction, abduction of the fingers and thumb including opposition is intact. The fingers are warm and well perfused with good capillary refill. Full range of motion of the elbow without pain. Full range of motion of the shoulder without pain. Clavicles are nontender bilaterally.
All other joints demonstrate normal exams
Emergancy Ortho: Elbow
The Elbow
ATRAUMATIC ELBOW PAIN:
Most often this can be diagnosed in 30 seconds with point tenderness and resistance of wrist flexion and extension. This is because the most common tendonitis or overuse injuries at the elbow are actually the insertion of the common flexor and common extensor tendons of the wrist and hand. Medial epicondylitis (i.e. Golfer's elbow) is tenderness at the medial epicondyle and pain there with resisted elbow flextion, while lateral epicondylitis (Tennis elbow) is pain at lateral epicondyle with palpation and resisted wrist extension. No x-rays are required and wrist splinting with pressure bands at the proximal tendon with ice and NSAIDs are the treatment of choice. Of course, the biceps and triceps tendons can have tendonitis and this is demonstrable on exam as well. There will be tenderness of these tendons and pain with resisted movement. The triceps is responsible for elbow extension and the biceps brachii can be isolated by having the patient flex the elbow and supinate against resistance (I grasp their hand like a handshake to add resistance). Sometimes olecranon bursitis results without trauma or very mild trauma and is again easy to see, palpate, and diagnose. Much consternation arises with aspiration of these bursa or not, so I will duck out of the debate and say that rarely would I aspirate because those whom I am concerned have a septic bursa look like there could be overlying cellulitis and I don't want to seed a sterile inflamed bursa. Call your local orthopedist for advice.
What to document:
R/L handedness and any repetitive movement in occupation or recreation that could cause the symptoms.
Specific location of the tenderness and what elicits the pain as a epicondylitis can be subtlety different from a biceps or triceps tendonitis.
Always the vascular status distally (i.e. radial pulse)
Always the neuro function at the joint and distally.
What to do:
Test for elbow pain with wrist flex/extension. As mentioned the common flex/ext tendons insert at the elbow.
X-rays are rarely absolutely necessary but do add to the diagnosis as sometimes you could catch an avulsion fracture
Start NSAIDs and ice. This usually will dramatically decrease pain. I like to have patients freeze small paper cups of water and rub them on the areas of pain.
What not to miss:
A full tear of the distal biceps. Flexion can be achieved with the brachioradialis so assess in full supination and with resisted supination compared to the contralateral side. Long term tendonitis or medications can weaken the tendon making the full tendon tear a relatively atraumatic event.
Same can be said for triceps tendon tear. Be sure to take gravity out of the equation when testing the triceps strength. Thankfully this is the only extensor.
Example PE for epicondylitis:
Musculoskeletal: The *** elbow is exquisitely tender over the *** epicodyl. Full flexion and extension of the elbow. Wrist flexion and extension exacerbates the pain but is intact. No tenderness over the olecranon or triceps brachii tendon. No swelling of the olecranon bursa. The shoulder is not swollen or deformed on inspection and range of motion is full. There is no bony tenderness along the radius or ulna distally. Sensation intact over the lateral deltoid and down to the fingertips. Positive radial pulse. Normal range of motion and 5+ strength to flexion and extension of the wrist and elbow. Fingers are warm and well perfused and sensation intact.
A review of the bony features of the elbow.
TRAUMATIC ELBOW INJURY
Most commonly from a FOOSH (fall on outstretched hand) injury, the radial head fracture is the winner of the most common injury in this joint. With the aforementioned mechanism and tenderness over the radial head (and pain with pronation/supination), have a low threshold to diagnose with occult fracture (even if one is not seen on plain films). As seen below, the presence of a posterior fat pad or sail sign indicates swelling (in this case bleeding) into the joint capsule and could indicate a radial head fracture and thus should be treated as such until proven otherwise. By way of review, a posterior fat pad seen on lateral films is never normal and an anterior fat pad can be normal but shouldn’t be a large triangle like a sail anteriorly. Little did I know, but you can also get a radial head-capitellum view plain x-ray in addition to standard views to pick up a few more radial head fractures not seen on initial films. Plain films are not perfect so splint all your patients with a strong likelihood of radial head fracture by history, exam, and/or x-rays in a long arm splint at 90 degrees flexion down to the wrist to prevent pronation and supination. These patients should be seen by ortho urgently as they might need surgery.
Radial head capitellum view, aka 45 degree radial head view from http://www.wikiradiography.net/page/Imaging+Radial+Head+Fractures
Other traumatic injuries include olecranon fracture and elbow dislocation. Both are easily seen on x-rays. The former occurs usually with a fall directly onto a flexed elbow (the x-ray finding and exam is obvious) and the latter takes substantial force to dislocate this relatively stable joint (and it takes a fair amount of force to reduce as well).
I have found the technique to the right to be the most effective, but if less muscle mass the other techniques would work.
What to document:
R/L handedness
Mechanism of injury
Radial pulse and capillary refill distally
Neuro exam of the wrist and hand
Bony tenderness or deformity of the medial/lateral epicondyl, olecranon, radial head and down the radius and ulna to the wrist.
What to do:
Splint fractures and suspected fractures at 90 degrees flexion. Per usual check and document neurovasc status after application
Provide pain relief up to procedural sedation for elbow reduction
What not to miss:
Test the radial, ulnar, and median nerves separately (see above) as they all cross the joint and could be injured in trauma
Feel radial pulse distally and consider an Allen test for possible ulnar artery injury.
Always think potential compartment syndrome and look for signs as well as warm patient of symptoms and when to return for a recheck.
Example PE for elbow trauma:
Musculoskeletal: The *** elbow has *** deformity. There is bony tenderness over the ***. Flexion and extension of the elbow is limited to ***. Strong wrist flexion and extension. No swelling of the olecranon bursa. The shoulder is not swollen or deformed on inspection and range of motion is full. There is no bony tenderness along the middle and distal radius or ulna. Sensation intact over the lateral deltoid and down to the fingertips including the palm and dorsum of the hand. Positive radial pulse. Normal range of motion and 5+ strength to flexion and extension of the wrist and fingers including finger adduction and abduction with good opposition of the thumb. Fingers are warm and well perfused and sensation intact.
Emergency Ortho: Shoulder
The Shoulder
ATRAUMATIC SHOULDER PAIN:
By far and away this is going to be shoulder impingement syndrome which is really a catch all for subacromal bursitis and/or supraspinatus tendonitis. This is further discussed below. One hallmark for this is pain at night sleeping on the affected side and exam shows pain with anything that decreases the space in the subacromial area (i.e. empty can and Hawkins maneuver). Other subtle diagnoses to consider would also include proximal biceps tendonitis with pain in the same area but instead a Speed's test is positive or just resisted elbow flexion and supination (remember the biceps is the primary supinator) causes pain. If there is bruising and a Popeye arm deformity consider a biceps muscle or tendon rupture. Biceps tendon rupture can be proximal or distal so a patient may present with anterior shoulder pain and have the muscle deformity there. Patients can also have tendonitis of any of the other rotator cuff muscles (remember your SITS muscles), but this is much less common. Mostly document good movement of these muscles to assess for adhesive capsulitis. This can be done with the lift off test and resisted external rotation with arms at sides and elbows at 90 degrees. A full list of special tests can be found on Medscape.
What to document:
R or L hand dominant (arthritis/bursitis) more likely on overused side
Pain at night and with overhead movement, think impingement
Any biceps deformity or pain on exam could indicate a biceps etiology
Speed's test is for proximal biceps tendonitis and should be done while palpating the proximal tendon in the bicipital groove. It can also indicate a labral tear as this is where the long head of the biceps tendon inserts.
Empty can test decreases subacromial space and is for impingement syndrome. A painful Neer's impingment or Hawkin's test do the same.
Test internal and external rotation of the shoulder as well with the lift off test (dorsum of hand on low back and lifted off) and the resisted internal rotation with the arm abducted and elbow at 90 degrees.
Feel a radial pulse and test elbow and wrist flexion/extension
A frozen shoulder (adhesive capsulitis) will have decreased ROM passively, many other etiologies can have decreased active ROM due to pain.
What to do:
A sling is fine in the short term but can lead to frozen shoulder particularly in the elderly.
Encourage early ROM exercises like pendulum swing.
Often pain will be chronic and need a PT referral, inform patient to f/u with PCP or orthopedist if not improved with conservative measures.
Strengthening of the rotator cuff muscles is helpful in many conditions so as long as not worsening pain with the exercises start rotator cuff muscle strengthening. This is a reasonably good educational video for patients and providers to treat impingement syndrome.
This is another great guide for shoulder rehab that you can print and send home with patients.
What not to miss:
A complete rotator cuff tendon tear. This will usually be the supraspinatus muscle and patient will not be able to abduct the first 15 degrees. They may compensate with shoulder hiking and will have a positive arm drop.
Biceps pathology such as a tear that may delay appropriate diagnosis and treatment.
Any neurologic or vascular injury.
Of course, any medical diagnosis (such as ACS) that might mimic or have associated shoulder pain. A good history and PE should clear this up so be thorough.
TRAUMATIC SHOULDER INJURY:
Be sure to get a Y view as pointed out by this great article on posterior dislocation on LifeInTheFastLane.com
Hard to miss a glenohumoral dislocation or humoral neck fracture (BTW it's the surgical neck not the true humoral neck) on x-ray. Except for a posterior dislocation which can be missed on just an AP view (see image right). Also because there are a bunch of different ways to reduce a shoulder, I won't go into the debate here, but just know if there are multiple ways to do something there is no one best way so find a technique and get good at it. Subtleties to these exams include documenting sensation over the lateral deltoid which shows the axillary nerve is functioning as it is often damaged with dislocation or fracture. Of course, always document neuro and vascular status distally as the brachial artery and the arm nerves run close to the humerus. A clavicle fracture is the most common of all the traumatic shoulder injuries and should be evident on exam and confirmed on x-ray. I've never met one that couldn't go home for outpatient follow-up but check to make sure it's not an open fracture or the skin is tented and blanching and soon to be an open fracture. Those would need immediate surgical reduction. An AC joint separation, can be difficult to pick up on plain films so consider looking at the contralateral side for comparison and if mechanism and exam is strongly indicative my be a grade I. Knowing the grades of AC joint separation not all that important as you could sling them all and send them to ortho outpatient.
Having a quick neuro exam of the hand/fingers is a good way to ensure proximal peripheral nerve function is okay. You can make up your own or memorize this quick exam of the nerves of the arm
Radial nerve: sensation = dorsal hand, webspace between thumb and index finger; action = elbow/wrist/finger extension
Median nerve: sensation = radial border of the index finger; action = thumb abduction (thumb to index finger)
Ulnar nerve: sensation = ulnar border of the 5th finger; action = fifth finger abduction (spread the fingers)
Musculocutaneous nerve: sensation = mid lateral forearm; action = elbow flexion with supination (to isolate the biceps brachii)
Axillary nerve: sensation = over insertion of the deltoid muscle; action = shoulder abduction
Bonus: pinch the thumb on the fifth finger to assess median and ulnar nerve motor function at the same time!!!
What to document:
Complete neuro exam: discussed above
Vascular exam including distal pulses and capillary refill.
Bony tenderness or deformity (compare to contralateral side). This should include at a minimum cervical spine, spine of the scapula, clavicle, AC joint, acromium
Soft tissue deformity, or lack thereof. Classically the squaring of the deltoid with anterior dislocation.
Active and passive ROM. If any intervention such as reduction is performed document ROM before and after.
What to do:
Get X-rays duh! Probably not a good idea to try to reduce a supposed dislocation that is really a fracture.
Treat for pain. Sometimes moving the joint for radiographs and of course interventions such as reduction need appropriate pain control up to procedural sedation.
Call for expert advice in anything that you don't routinely handle. My rule of thumb is call a consultant surgeon for anyone that is going to eventually need surgery.
What not to miss:
Nerve or vascular injury. Particularly fractures can lacerate important structures like an artery. The axillary nerve (see below) is the most common nerve injury from dislocation. It provides sensation of the lateral deltoid. Document sensation here before the patient goes home (that means before and after reduction).
Secondary injury such as head or neck. If there is enough force to dislocate or fracture then perform a full physical (such as an ATLS secondary survey) to look for concomitant injuries.
Example documentation of the PE:
Musculoskeletal: The *** shoulder is *** swollen or deformed on inspection. The range of motion is full/limited to *** because of the pain. There is good abduction without shoulder hiking and no arm drop when compared to the contralateral side. There is *** tenderness of the clavicle, a.c. joint, or spinous scapula. There is *** tenderness inferior to the acromion in the area of the supraspinatus tendon and bursa. Empty can test is ***. Hawkin's test and Neer impingement test is ***. Speed's test is ***. There is *** internal and external rotation as tested by lift off and resisted external rotation with arm in adduction. Sensation intact over the lateral deltoid and down to the fingertips including the palm and dorsum of the hand. Positive radial pulse. Normal range of motion and 5+ strength to flexion and extension of the wrist and elbow. Fingers are warm and well perfused with good capillary refill.
How to Approach Traveler’s Fever
Is that even a term? I think I just made it up. Oh well, you’ll get the idea if you keep reading.
Does your patient have a fever after traveling? How soon (or late) after traveling do you worry that the fever may be related to an exposure abroad? Of course, the answer is very complicated with literally thousands of diseases worldwide to worry about. Thankfully, most patients from the US and other developed countries have been vaccinated in childhood to protect against measles, tetanus, and the like. Also, many people will visit a travel clinic to receive more vaccines and sometimes prophylactic medicines so it is very important to ask about all childhood and recent vaccines as well as any other medications they were given as prophylaxis.
Generally speaking, in regards to incubation periods, usually we should consider possible exposures abroad as the culprit for any fever that begins within 1-4 weeks of travel. Of course, my first go-to is the CDC Traveler’s Health website where there is a wealth of information including disease endemic to the area where the patient traveled as well as the incubation times for these disease. There, when you can select information for clinicians on a wide range of topics including recommendations and warnings about particular countries. Your first step should always be, check the CDC. If the country is listed in the triage note, I often look at the CDC page even before entering the room to get my differential diagnosis going.
Mostly we are going to talk about the mosquito-vector diseases here.
Fever in a recent traveler is a very difficult diagnosis to make, in my opinion, and I find it frustrating that patients often expect the US based ED to know all the disease presentations from world-wide travel. For me, I have to write this stuff down as reminders (welcome to my peripheral brain.)
MOSQUITO-BORNE ILLNESSES
Of course, the best treatment is prevention. To safeguard against these you should always have good mosquito protection when traveling to tropical areas. Common sense says to wear pants and long sleeves, use netting if needed, and avoid the dusk and dawn feeding times, but as far as bug spray is concerned the DEET options are still the best. The distribution of the following diseases is generally around the equator illustrated in the map above (which also includes Lyme and other tick-borne illnesses discussed further below and aren’t commonly considered in traveler’s fever cases).
The list of illnesses with a mosquito vector includes the following:
Chikungunya Virus (CDC Chikungunya Virus, WHO Chikungunya Virus)
Dengue Virus (CDC Dengue, WHO Dengue)
Eastern Equine Encephalitis Virus (CDC Eastern Equine Encephalitis)
Japanese Encephalitis Virus (CDC Japanese Encephalitis Virus, WHO Japanese Encephalitis Virus)
La Crosse Encephalitis (CDC La Crosse Encephalitis)
Malaria (CDC Malaria, WHO Malaria)
St. Louis Encephalitis (CDC St. Louis Encephalitis)
West Nile Virus (CDC – NIOSH – West Nile Virus)
Yellow Fever (CDC Yellow Fever, WHO Yellow Fever)
Zika Virus (CDC – NIOSH – Zika Virus)
Five different human malaria Plasmodium species and their life stages in thin blood film (Source: K. Silamut and CDC).
Thankfully, a lot of these are rare, and a major clue to the presentation lies in the names that have the word “encephalitis.” This means that a major feature is just that - encephalitis - a sick patient with AMS or other neuro symptoms. In general, these are not going to be the patients that walk into your ED waiting room with a fever, wondering if it is a disease picked up on their last trip to the Caribbean. For now, being rare and fairly dramatic in presentation, we will skip these.
In terms of the common mosquito-borne illnesses, malaria ranks at the very top because it is generally more severe, and because it is treatable (besides supportive care). Most healthy travelers will recover from all of these disease and usually can be treated outpatient. Malaria is also, generally easier to test for by looking at a thin smear. Most labs can handle this in an hour or two. I’ve even had an excited lab tech call me about the blood smear, and I even went to the lab to check it out myself!
Therefore, think malaria first when considering a fever in a traveler to a tropical or endemic area because this can and should be treated. There are tests for the other diseases listed but it may be unnecessary to send tests for chickungunya and zika due to milder symptoms and low complication rate. There may be a lower threshold to send tests dengue but actually most people are asymptomatic with the disease.
Now, on to the most common mosquito vector diseases
Malaria has a distribution all around equator just like dengue, more in sub-Saharan Africa.
Prophylaxis: Good if taking as recommended, but not perfect. Therefore, you must consider in patients who may have missed some doses or even taking it correctly as it is not 100% protective.
Tests: Send a thin smear to look for malaria, high sensitivity to rule out the disease but not perfect either. Start with this test. Then add thick smear, blood cultures, and any other tests for disease that enter your differential (like Dengue). If thin smear negative, usually you can discharge a well-appearing patient. Malaria usually more severe than the following diseases so being well enough to go home with malaria has a good prognosis.
Treatment: Here I would say just look it up and/or ask your friendly ID doc who would likely love a consult for this disease. For tests, just remember ACT (artemisinin combination therapy, commonly lumefantrine/artemether). This is usually oral, but there is an IV version if sick (vomiting, hypotensive). Usually patient can be discharged on 3 days of oral treatment, 6 if high resistance in the area of travel. Quinine and doxy is older option.
Disposition: Most people do not become ill enough to need hospitalization. Obviously, there will be exceptions based on age, baseline health, etc. Thankfully, the most common of the species (falciparum) does not go onto cause recurrent disease, although people can be reinfected, whereas some other species (vivax & ovale) do reside in the liver and can be recurrent. Return precautions and ID follow-up is a must.
Dengue has the same distribution as malaria, but more in Southeast Asia. The key is to think of both malaria and dengue because they have so much overlap
Prophylaxis: None, use mosquito protection
Best test is IgM/IgG, but often a send out lab that can take a week or so.
Symptoms: Muscle aches and headache common. Hemorrhagic shock is rare and more common in repeat infections.
Treatment: Supportive
Disposition: Usually, home. The shocky patients will obviate the need for admission.
Chickungunya has a smaller but similar area of tropical distribution. For more, scroll down.
Prophylaxis: None, use mosquito protection
Tests: This is self-limited and diagnosed primarily on symptoms and exposure alone. Testing often not needed.
Symptoms: Flu-like symptoms as with the other but joint pain (which is usually generalized and can be severe) is distinguishing feature.
Treatment: primarily NSAIDS for arthralgias and supportive care.
Zika has the same as above in terms of geographical spread. May test in pregnancy.
Prophylaxis: None (but I bet you could make billions if you invented one)
Tests: Also usually not done but because zika has gotten a lot of press lately there may be some concerned pregnant patients in whom you might consider testing. Otherwise test is not needed
Symptoms: Flu-like illness
Treatment: Supportive care
Yellow Fever is also a tropical disease. Thankfully, the CDC says, “Yellow fever is a very rare cause of illness in U.S. travelers” which means we can probably stop there, but for completeness sake.
Prophylaxis: None
Tests: Essentially none as it is diagnosed based on other lab findings, symptoms, and travel to Africa or South America.
Symptoms: Per the CDC “Illness ranges from a fever with aches and pains to severe liver disease with bleeding and yellowing skin (jaundice).
Treatment: None, nothing to treat or cure the infection. Supportive care and managing complications is the task. The “yellow” refers to jaundice so assessing and treating potential liver failure is needed.
Don’t forget “normal” common fever causes. Patients could return with influenza or other common viral illnesses. Of course, always look for clues of more dangerous illnesses like encephalitis or meningitis and treat any patient in hemorrhagic or septic shock (rare but possible with dengue and malaria) aggressively with early ID intervention.
Bottom line: Test travelers to endemic areas with fever for Malaria first. A thin smear is fairly sensitive and rapid. If this is negative and the patient looks well, discharge home is a reasonable option. Dengue is usually a send-out test, most infections are mild, and you will know when to admit because rarely the patient will be in hemorrhagic shock. Dengue, chickungunya, and zika all are usually flu-like illnesses that just need supportive care. Also, remember the “normal” cause of fever we see and work-up all the time in the US. Fever after traveling does not mean a rare disease only.
Of course, other bacterial and parasitic causes of fever in travelers include leptospirosis, typhoid fever, trypanosomiasis and schistosomiasis all of which need a separate discussion (to come).
Chikungunya!
It's spelled how it sounds, yet I still have trouble spelling it. The name, chikungunya, is from an African dialect meaning "stooped walk" or "that which bends up" referring to its primary manifestation of joint pain. I hadn’t even heard of the disease until several years out of PA school, but after working in an ED that saw plenty of immigrants from the Caribbean Islands, I quickly learned that this is generally not a dangerous disease and mostly treated symptomatically. That being said, is is good to have some idea of some basic pathophysiology and possible complications. Here's a reminder of the highlights of the disease...
Endemic in some parts of West Africa, chikungunya has now been found on every other continent including the Americas. Even though experience was in patients who returned from tropical areas (the first cases in the Caribbean islands was confirmed in 2013 and in Florida in 2014), it is technically not defined as a tropical disease because it has spread to places like Italy in 2007.
Chikungunya is primarily transmitted by mosquito vectors, extremely rarely by blood products or maternal-fetal transmission.
The incubation period is usually 3-7 days (range of 1-14 days) before abrupt onset of fever and malaise.
Symptoms: Acute illness is about 7-10 days
Fever may be over 39 C for 3-5 days
Polyarthralgias (usually symmetric and distal more than proximal) 2-5 days after fever. Pain can be quite intense and disabling. Joint effusions can be present.
Maculopapular rash in 1/2 to 3/4 of patients usually on trunk and limb, sometimes puritic (25-50%)
Conjunctivitis sometimes occurs
Lymphadenopathy can occur
Severe complications can occur in the elderly and chronically ill. These can include organ failure (respiratory failure, renal failure, hepatitis, cardiovascular collapse), but watch especially for neurologic findings - meningoencphalitis most common, also flaccid paralysis, Guillain-Barre, cranial nerve palsies as well.
Diagnosis
Most diagnosed by fever/arthragias with travel to endemic area and mosquito exposure
Tests are available if needed - RT-PCR of chikungunya virus RNA if patient presents 1-7 days after symptom onset and if >7 days, chikungunya virus serology by ELISA or IFA (although I’ve never sent off any of these tests)
If patient could have chikungunya based on mosquito exposure in endemic areas also consider dengue and Zika virus.
There are many other mimics, with the most common being viral illnesses like parvovirus B19
Treatment:
There is no antivirals for chikungunya!
Supportive care - rest, acetominophen, NSAIDs, etc
Caution with using aspirin and NSAIDs in patients with dengue
Prevention is the key! That means avoiding mosquito bites.
If you really want to take a deep dive into chikungunya, check on its geographic distribution, as well as get information for providers and patients, of course, check out the CDC.
HHS
HYPEROSMOLAR HYPERGLYCEMIC STATE
While DKA is more commonly seen in patients <65 years old, HHS is most common in older patients (>65 years). Although rate of hospital admissions for HHS are typically lower than DKA, the mortality rates are about 10x higher. HHS differs from DKA in that it doesn't have the "A" for acidosis. The criteria for HHS can be found in the name:
H – hyperglycemia (glucose > 600 mg/dl)
H – hyperosmolarity (serum osm >320 mOsm/kg)
Patients with HHS can have very high glucose levels, and in some ways, mimic DKA patients in their initial clinical presentation. Symptoms of HHS include excessive thirst and urination, fever, AMS, vision loss, and seizure/coma. It is important to note that, unlike DKA, HHS typically does NOT present with abdominal pain and is more likely to have neurologic abnormalities such as focal weakness, sensory changes, and seizures/coma.
These patients are usually in profound fluid deficit, even more so than those in DKA. The fluid deficit for HHS can be as much as 5-20 liters. As mentioned before – you can use NS, but LR or plasmalyte would be a better option for fluid resuscitation given the large volumes needed.
Treatment for HHS is essentially the same as that for DKA except with a few small key differences:
The patient may require up to 12L of fluid over a 24-26 hour period
D5 should be added to the IVF when BG reaches 250-300
The target to correct the effective osm is 3 mOsm/kg/hr
Make sure you do not overcorrect this too quickly or else you will run the risk of causing cerebral edema
And don’t forget to keep an eye on those electrolytes!
Points to remember:
No ketoacid accumulation, glucose often >1000, plasma osmolality elevated as high as 380
Can present with neuro abnormalities and coma
Same precipitating factors as DKA
Treatment: fluid replacement and electrolyte repletion:
0.9% NS followed by 0.45% saline to replace typical volume loss of 8-12L. Half of volume over 12hrs then the other half over 24hrs. Could consider other balanced solutions like PlasmaLyte or LR.
K, Mg, Phos all monitored and treated as in DKA
Insulin drip will be needed
If there is no neuro deficit, even patients with glucose >1000 and not acidotic are not technically in HSS and could even be treated with IV fluids and subcutaneous insulin.
DKA
Diabetic ketoacidosis is the result of two problems: insulin deficiency and excessive release of counterregulatory stress hormones. Counterregulatory stress hormones include glucagon, cortisol, growth hormone, and catecholamines – they work to oppose the actions of insulin and increase the energy availability for the body (aka, gluconeogenesis and glycogenolysis). When the body is under extreme stress, these hormones drive up blood sugar levels. This, paired with a suboptimal insulin response, can lead to DKA.
While diabetic ketoacidosis is characteristically associated with Type 1 diabetes, it can be seen in Type 2 diabetics under conditions of extreme stress (such as serious infections, cardiovascular emergencies, or trauma). The triggers for DKA are easy to remember with the 5S rule:
Sepsis
Surgery
Sugars (missed insulin dose)
Stress
Substances (alcohol, drugs)
Symptoms of DKA include excessive thirst and urination, delirium/dizziness, dehydration, ketotic breath, and abdominal pain. And remember, just because the patient does have “diabetes” in their past medical history, doesn’t mean you should cross DKA/HHS off your differential. Diabetes can certainly remain undiagnosed if the patients isn’t following up with their PCP on a regular basis.
So, how do we diagnose DKA? The name says it all – glucose is elevated, pH is low, and ketones are up. However, there are actual diagnostic criteria – four to be exact. Fortunately, there is an easy acronym to remember these criteria as well: DKAA
D – diabetes (glucose must be >250 mg/dl)
K – ketonemia (measure with a UA and serum beta-hydroxybutyrate)
A – acidosis (pH must be <7.3)
A – anion gap (serum bicarb must be <18)
If your patient does not meet ALL four criteria, they do not have DKA.
The name says it all, but there are actual diagnostic criteria. Glucose is elevated, pH is low, and ketones are up. In treating, you need to correct the acidosis caused from generating all those ketone bodies generated from ketolysis due to the inability to burn glucose. Beta-hydroxybutyrate is actually the most common ketone body (there are multiple) with acetoacetate being less common. Acetoacetate (acetone) triggers the urine ketone test so it is possible to be in DKA with negative urine dip for ketones, but that would probably only be very early. For serum testing just go with beta-hydroxybutyrate serum levels if you can.
Beta-hydroxybutyrate is actually the most common ketone body (there are multiple) with acetoacetate being less common. Acetoacetate (acetone) triggers the urine ketone test so it is possible to be in DKA with negative urine dip for ketones, but that would probably only be very early. For serum testing just go with beta-hydroxybutyrate serum levels if you can.
The severity of DKA is determined by the pH since the glucose can be variable. This study showed that mild DKA could be treated with aspart subcutaneous insulin just as well as IV insulin. Of course, if the patient is exhibiting neurologic symptoms like AMS (drowsy/stupor), then their condition is more severe and potentially even life-threatening. Also, consider HHS if patient has an AMS and hyperglycemia but their pH is normal.
In treating, you need to correct the acidosis caused from the ketolysis that is a result of the body’s inability to utilize its glucose. Start with the following:
Isotonic fluid replacement – HYDRATE. HYDRATE. HYDRATE. These patients can have a water deficit of as 5-10L so don’t be shy with the IVF. It’s good to start with LR or PlasmaLyte because large amounts of NS (4-5L) can add free H+ to cause a hyperchloremic metabolic acidosis.
But wait! Make sure you check their electrolytes first, especially potassium. Patients in DKA typically have a substantial potassium deficit due to glucose-induced osmotic diuresis. However, their lab values usually don’t reflect that. In acidosis, the body tries to compensate by driving H+ into the cell in exchange for K+. Because of this, potassium can appear to be normal or falsely elevated at presentation. If their potassium is <3.3, make sure to replete before initiating fluids and insulin as this will drive potassium back into the cells.
Insulin at 0.1 units/kg/hr - stop drip when AG closes, might even need to continue when glucose <200 but add Dextrose (D5 or D10) to the fluids.
Potassium will fall: easiest rule to remember was discussed in the July 2017 EM:RAP episode as the 3.5 to 5.5 rule. If potassium is above 5.5, just start the insulin infusion, if between 3.5-5.5, add K (10-20 meq) to the fluids. If it is less than 3.5, hold the insulin, supplement the K and start the insulin later. Strictly speaking, according to more universal guidelines:
if K <3.3 replace K 30 min prior to insulin
if K 3.3-5.0 replace K during insulin drip
Phos replacement if below 1mg/dL
Mg replacement if low or symptomatic
Bicarb not recommended
Monitor the patient's mental status, respirations, AG, glucose, bicarb, and K closely, usually every hour initially. Remember, you're not done when you start the insulin drip. These are ICU patient's that need one-to-one nursing with at least q1hr glucose/lab checks.
Points to remember:
DKA Triad - hyperglycemia, anion gap metabolic acidosis, and ketonemia (look for beta-hydroxybutyrate)
DKA can be precipitated by noncompliance with insulin, trauma, infection, pregnancy, and other stressors and occurs in type I or type II DM. Look for, and correct, the precipitating cause, which might just be diet/med noncompliance.
Treatment: correct fluid deficit, acid-base disturbance, and electrolyte imbalance, administer insulin, and treat the underlying cause
Anaphylaxis
Yeah, about the only thing we care about in the ED allergy related is anaphylaxis. Sure, hundreds of patients will enter your ED with weird rashes, obvious hives, bug bites, bee stings, and poison ivy that never even come close to the definition of an emergency ("but it is to me!" your patients will say). Yet, the only thing you are really responsible for doing in these cases is make sure you're not missing is....Anaphylaxis. That's why I always make sure to include a negative ROS that includes those questions that pertain to true anaphylaxis. But what is anaphylaxis really???
The America Academy of Allergy and Asthma (yes, the AAAA) says, "Anaphylaxis (an-a-fi-LAK-sis) is a serious allergic response that often involves swelling, hives, lowered blood pressure and in severe cases, shock. If anaphylactic shock isn't treated immediately, it can be fatal."
Merriam-Webster writes, "hypersensitivity (as to foreign proteins or drugs) resulting from sensitization following prior contact with the causative agent."
The National Institute of Allergy and Infectious Diseases most correctly states, "Anaphylaxis is a serious allergic reaction that involves more than one organ system (for example, skin, respiratory tract, and/or gastrointestinal tract). It can begin very rapidly, and symptoms may be severe or life-threatening."
The most salient points being, 1) it is life-threateningly serious, 2) must involve more than one organ system, and 3) can be very rapid. Therefore, it requires expedient recognition and treatment.
We all know that the definative treatment is epinephrine, but unfortunately since we give it so infrequently (like more often in coding dead patients), sometimes we are slow to pull the epi-trigger. This, of course, could be a fatal mistake, so here is a quick overview.
The starting dose for epiniphrine (the epinephrine autoinjector dose) is 0.3mg deep IM. I suggest you encourage your ED to carry autoinjectors because it can take a surprisingly long time for your nurses to draw this up.
For patients with severe anaphylaxis give 0.5mg epinephrine IM in the thigh (best absorption here).
If the patient still needs epinephrine (multiple IM doses needed) and you need an epinephrine drip. Recommended IV epinephrine is to start at 1-4mcg/min or 0.1mg over 5 min.
Unfortunately, an epi drip can be similarly difficult to obtain from pharmacy. A trick of the trade can be found at ALiEM here to make a "dirty epi drip."
Get 1mg of epinephrine (from code cart)
Inject this 1mg of epi into 1,000 mL normal saline bag which = concentration of 1 mcg/mL
Rune wide open until symptom response and/or patient stabilizes
Wide open administration of a “dirty” epinephrine drip results through 18G IV cathaeter is about 20-30 mcg/min when administered wide open. This can be titrated down when the symptoms improve. 1ml per min (60ml/hr) would be a 1mcg per min recommended starting dose.
Give an H1 blocker (like Benedryl) and an H2 blocker (like Pepcid) to help urticaria although no benefit in anaphylaxis has been demonstrated.
Glucocorticoids similarly have not been of proven benefit but routinely given.