The Easy-IJ: Rapid Venous Access in Critical Care
Stop Fiddling with the CVC Kit: Why the "Easy-IJ" is Your New Resuscitation Best Friend
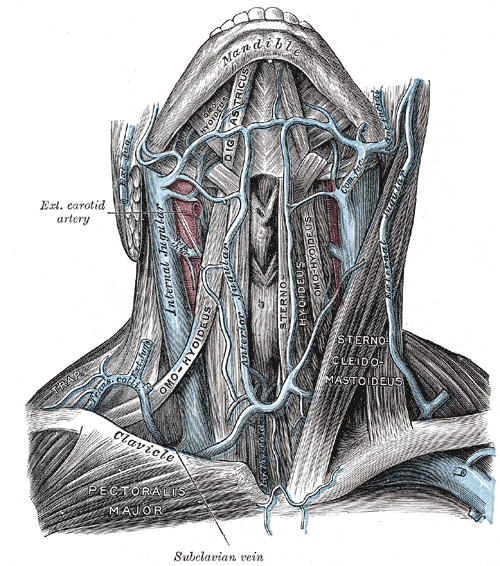
Zervikale Venen von vorne in der anatomischen Zeichnung von Henry Gray. Public Domain
We’ve all been there: a critically ill patient is crashing, the nurses have already failed multiple peripheral IV (PIV) attempts, and the clock is ticking. While your instinct might be to reach for a triple-lumen central venous catheter (CVC), stop and consider the "Easy-IJ"—the practice of placing a single-lumen PIV catheter into the internal jugular (IJ) vein under ultrasound guidance [1-4].
It is fast, safe, and backed by a growing mountain of evidence that can help you defend this practice to even the most skeptical department administrator.
Speed: Because Minutes Matter
In a resuscitation, time is the only currency that counts. While a full CVC can take up to 20 minutes to set up and complete, the Easy-IJ is a speed demon. Studies show median access times for the Easy-IJ range from a mere 3 to 5.3 minutes. By skipping the unnecessary venous dilation and extensive sterile draping required for central lines, you get life-saving fluids and meds into your patient significantly faster [1, 2, 4, 5].
Little Vessel, Low Risk
If anyone gives you grief about "putting a peripheral line in a central vessel," hit them with the data:
Zero Pneumothoraces: Across multiple studies of the Easy-IJ, there were no reported pneumothoraces or arterial punctures [2,4].
High Success Rates: The IJ is a large, superficial target that is easily identified via ultrasound, even when the patient is hypovolemic [1, 2]. Success rates for this technique range from 55% to 100%, with many clinicians hitting it on the first attempt [1,6].
Reduced Infection Risk: Because you aren't using a guidewire (in the traditional sense) or a long-term dwelling catheter, the risk of bloodstream infections may actually be lower than a CVC [6].
You Already Know How to Do This!
One of the best parts of the Easy-IJ is the flat learning curve. You are simply combining two skills you already possess: ultrasound-guided IJ identification and standard PIV insertion. In one study, even residents with minimal training—just a 15-minute lecture—were able to place these lines with a 97% success rate [2, 4].
For an even smoother experience, consider using guidewire-assisted PIV catheters (like the VeloCath or AccuCath). These devices use the Seldinger technique to navigate vessel anatomy, reducing the risk of the catheter dislodging—a common headache with shorter PIVs in deep vessels [1, 6, 7].
Defending the Practice
When the "policy police" ask why you didn't follow full central line sterile precautions (BIOPATCH, full drapes, etc.), point out that the Easy-IJ is a peripheral access point, much like an external jugular (EJ) line, which we’ve used for decades without such fanfare . It is a less invasive, cost-effective alternative that saves central lines for when they are actually needed for hemodynamic monitoring [1, 4, 5].
The Bottom Line:
Incorporating the Easy-IJ into your resuscitation toolkit is like using a wide-open highway instead of a congested side street; both get you to the same destination, but one allows you to move at the speed of the emergency without the roadblocks of a complex procedure.
Of course, I’m not the only one in favor of this approach to emergency IV access, as you can see from the references throughout this post. There are also great blog posts and literature reviews I encourage you to check out. Like this one,
Salim Rezaie, "More on the Easy IJ", REBEL EM blog, May 4, 2017. Available at: https://rebelem.com/more-on-the-easy-ij/.
References:
Little A, Jones DG, Alsbrooks K. A narrative review of historic and current approaches for patients with difficult venous access: Considerations for the emergency department. Expert Review of Medical Devices. 2022;19(5):441. doi: 10.1080/17434440.2022.2095904.
Kiefer D, Keller SM, Weekes A. Prospective evaluation of ultrasound-guided short catheter placement in internal jugular veins of difficult venous access patients. The American Journal of Emergency Medicine. 2016;34(3):578. doi: 10.1016/j.ajem.2015.11.069.
Costantino TG, Kirtz JF, Satz WA. Ultrasound-guided peripheral venous access vs. the external jugular vein as the initial approach to the patient with difficult vascular access. The Journal of Emergency Medicine. 2010;39(4):462. doi: 10.1016/j.jemermed.2009.02.004.
Zitek T, Busby E, Hudson H, Mccourt JD, Baydoun J, Slattery DE. Ultrasound guided placement of single-lumen peripheral intravenous catheters in the internal jugular vein. WestJEM. 2018;19(5):808. doi: 10.5811/westjem.2018.6.37883.
Butterfield M, Abdelghani R, Mohamad M, Limsuwat C, Kheir F. Using ultrasound-guided peripheral catheterization of the internal jugular vein in patients with difficult peripheral access. Am J Ther. 2017;24(6).
Chai HS, Kim Y, Park GJ, et al. Comparison between internal jugular vein access using midline catheter and peripheral intravenous access during cardiopulmonary resuscitation in adults. SAGE Open Medicine. 2023;11. doi: 10.1177/20503121231175318.
Ash AJ, Raio C. Seldinger technique for placement of “peripheral” internal jugular line: Novel approach for emergent vascular access. WestJEM. 2016;17(1):81. doi: 10.5811/westjem.2015.11.28726.